Dr. Jan D’Haese Ghent University, March 2015
Use Of Dynamic Navigation For Dental Implant Surgery
INTRODUCTION
Although osseo-integration of dental implants is predictable1, thorough pre-operative planning is a prerequisite for a successful treatment outcome.2Anatomic limitations as well as prosthetic considerations encourage the surgeon to obtain a very precise positioning of the implants. Historically, standard radiographic imaging techniques (intra-oral and panoramic) were available for investigation of potential implant sites. Throughout the years, spiral tomography and computed tomography (CT) were often used as a diagnostic tool.3 These techniques provide a 2-dimensional cross section image of the desired implant location and enables a detailed bucco-lingual view of the dimensions of the jawbone. Nowadays, it is well known that 3-dimensional CT scan based pictures allow a more reliable treatment planning than when only 2-dimensional data are available.4 Transforming the CT scan images into a 3D virtual image can be achieved using computer software packages,5 allowing for a 3D viewing using Computer Aided Design (CAD) technology. For years, stereolithographic guided surgery seemed to be the golden standard in computer guided implant surgery. The technique has been well developed over the last years and several scientific reports have been published regarding accuracy, complications, survival and success6. Real-time navigation seems to be a valuable alternative to stereolithographic (static) guided surgery as it offers the clinician some advantages compared to the former technique. Using real-time (dynamic) navigation one can avoid the fabrication of a stereolithographic template resulting in a less expensive treatment. As navigation is considered as a dynamic guided surgery system, changes to the treatment planning (location and size of the implants, number of the implants, flap or flapless…) can be easily made intra-operatively.
CASE PRESENTATIONS
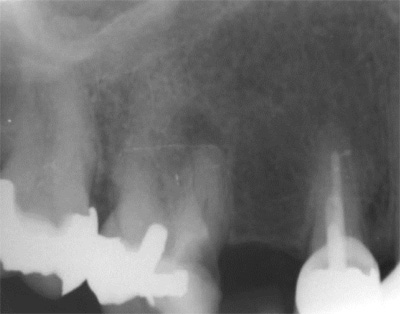
The first patient treated was a 59 year-old female consulting the dental office for replacement of two premolars in the maxilla, in locations 15 and 24 (Fig. 1, Fig. 2, Fig. 3). Patient was in good general condition and was a nonsmoker. Intraoral examination revealed numerous amalgam fillings and some metal-porcelain crowns (Fig. 4). Teeth 15 and 24 had to be extracted previously due to cariogenic process. Periodontal screening showed no signs of pathology. Treatment involved placement of 2 osseo-integrated implants in the edentulous regions of the maxilla.
The second patient was a 55 year-old male visiting the office to restore a recently extracted lateral incisor (Fig. 5, Fig. 6). He was a non-smoker, in good general health and not suffering from any systemic disease. Intra-oral examination showed several crowns in the maxilla and a residual root fragment in location 15 (Fig. 7, Fig. 8). Patient suffered from moderate periodontal breakdown. This periodontal condition has been present yet stable for several years.
For both of the patients, impressions of the dental arch were taken prior to implant installation using an irreversible hydrocolloid (Cavex CA37, fast set, Cavex Holland BV, Haarlem, The Netherlands) to fabricate a diagnostic cast (Fig. 9). This cast was used as a model for the molding of theNaviStent in order to have a perfect fit. The NaviStent serves as scanning template and is worn by the patient during the scanning procedure and the surgery. (Fig. 10).
Afterwards, the patient was sent to the CBCT and a scan was made with the NaviStent in place.
PLANNING PROCEDURE
A standard CBCT scan was performed according to the procedure outlined in the scanning protocol by Navident (Navident, Toronto, Canada).
The CBCT images were converted into a DICOM image (digital imaging and communications in medicine) and transformed into a 3-D virtual model using the Navident software system. The clinician who placed the virtual implants in the resulting 3-dimensional model also performed the actual surgeries. The potential locations for implant placement, and corresponding implant lengths and widths were planned in a prosthetically driven way. A distance of at least 3 mm from the neck of implant to the gingival zenith was applied, allowing the biological width to create a connective tissue contour around the abutments.
SURGICAL PROCEDURE
The surgery was performed under local-regional anaesthesia. Appropriate aseptic and sterile conditions prevented post-operative infections. During the operation, the NaviStent was placed over the remaining teeth (Fig. 11). The NaviStent was primarily fixated around the undercuts of the remaining teeth and additionally by application of a denture adhesive (prothese kleefcreme).
The osteotomies were prepared at maximum of 1500 rpm using the Navident navigation system to guide the drilling procedure in real-time by indicating the desired drilling pathway on the computer screen. Prior to the use of each new drill, a calibration process is performed (Fig. 12). No punching of the gingival tissues was performed prior to the preparation of the implant sites.
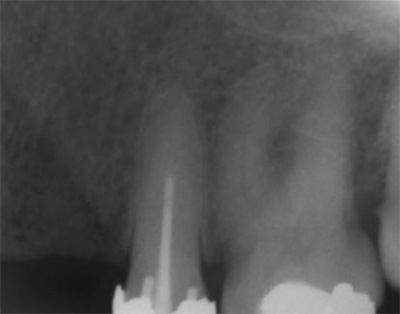
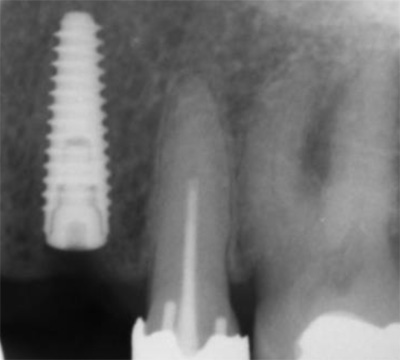
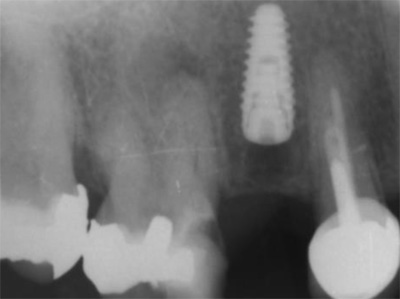
In the first patient, 2 Xpeed® Anyridge® implants (Megagen, Seoul, South-Korea) were installed. At locus 15; a 10 mm length and a 4 mm wide fixture was inserted whereas at locus 24 a 13 mm length and a 3,5 mm diameter wide implant was installed (Fig. 13, Fig. 14, Fig. 15).
In the second patient, a solitaire Xpeed® Anyridge® implant with a length of 10 mm and a diameter of 3,5 mm was placed at locus 22 (Fig. 16, Fig. 17). An Xpeed® Anyridge® implant consists of a nanolayer of calcium ions incorporated on the sandblasted, large-grit, acid-etched (SLA) implant surface. All the implants were inserted into the maxilla with a maximum insertion torque of 35 Ncm.
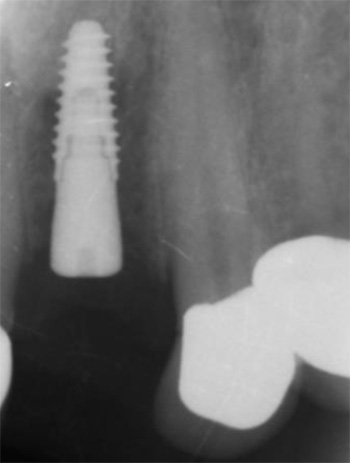
As the implant fixtures were also calibrated for use with the navigation system (Fig. 18), their exact position could also be tracked during insertion. This means that both implant preparation drilling and the implant placement process are tracked in real time. Depth of drilling and placement are guided by Navident using on screen visual representation and auditory cues to aid the clinician. Immediately after implantation, cover screws were placed onto the implants and hand torqued (Fig. 19, Fig. 20).
Postoperatively, patient received a prescription for antibiotics (amoxicilline 1000 mg, 2x/d, 4 days), for non-steroidal anti-inflammatory drugs (ibuprofen 600mg, 3x/d) and for a mouthwash (chlorhexidine 0,12%, 2x/d). After 1 week, a post-operative visit was scheduled. No signs of infection or inflammation were present as the healing went on uneventfully (Fig. 21, Fig. 22, Fig. 23).
CONCLUSIONS
In a one week postoperative follow up the patients reported no pain or swelling associated with the dental implant procedure. Further postoperative results are being tracked and reported as part of a qualitative study being done in cooperation with the University of Ghent. The potential of the Navident dynamic navigation system with regard to minimally invasive and accurate implant surgeries will be evaluated during this study.
REFERENCES
1. Albrektsson T, Dahl E, Enbom L, et al. Osseointegrated oral implants. A Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. J Periodontol 1988; 59:287–296.
2. Jacobs R, Adriansens A, Naert I, Quirynen M, Hermans R, van Steenberghe D. Predictability of reformatted computed tomography for preoperative planning of endosseous implants. Dentomaxillofacial Radiology 1999; 28,37–41.
3. Rothman SL, Chaftez N, Rhodes ML, Schwarz MS. CT in the preoperative assessment of the mandible and maxilla for endosseous implant surgery. Work in progress. Radiology 1988; 168:171–175.
4. Jacobs, R., Adriansens, A., Verstreken, K., Suetens, P. & van Steenberghe, D. Predictability of a three-dimensional planning system for oral implant surgery. Dentomaxillofacial Radiology 1999; 28:105–111.
5. Israelson H, Plemons JM, Watkins P, Sory C. Barium-coated surgical stents and computer- assisted tomography in the preoperative assessment of dental implant patients. Int J Periodontics Restorative Dent 1992; 12:52–61.
6. D’haese J, Van De Velde T, Komiyama A, Hultin M, De Bruyn H. Accuracy and Complications Using Computer-Designed Stereolithographic Surgical Guides for Oral Rehabilitation by Means of Dental Implants: A Review of the Literature Clin Impl Dent Rel Res 2012; 14: 321–335
Navident is cleared by the FDA for sale in the United States. Navident is approved for commercial sales and distribution in Canada by Health Canada. It has also received the CE mark; please contact ClaroNav.
Input the main text content for your module here.