Dr. Ricardo Henriques (Portugal, 2018)
Dynamic Navigation By Innovative Registration.
Background
3-D implant planning and mapping that plan to the real surgical environment are two important steps in implant rehabilitation.1,2 Misplaced implants can create difficult aesthetics, functional and biological problems and can result in implant loss.3–5
There are three ways to transfer a planned implant’s position into the real patient’s jawbone:
- mental navigation, so-called freehand navigation,
- static navigation using surgical templates,6 and
- dynamic navigation using a stereoscopic camera.7,8
The freehand approach is totally dependent on the surgeons’ experience, skills and mindset during treatment and creates the highest deviations compared to the other approaches.2
The usage of surgical templates provides a higher accuracy compared to freehand surgery, but has a few limitations, such as the inability to modify the plan once the surgical template has been manufactured. Surgical templates require longer drills which can make their use quite difficult or even impossible. Other concerns are irrigation issues and incompatibility with advanced surgical protocols.
Dynamic navigation is, at present, the most effective way to transfer the planned implant’s position to the real patient as it guides the surgeons’ motions using real-time feedback. It is especially useful to reduce flapped procedures with the advantage of improved soft-tissue healing, patient comfort and reduced bone resorption. Dynamic navigation allows planning modifications at any time, even during treatment, and can be used in cases with limited mouth opening or in combination with osseodensification drills.
The dynamic navigation concept using trace registration
In this approach, the patient’s jaw and the surgical drill’s location are being tracked by the navigation system’s tracking camera, using special tags affixed to them. To correspond between the physical patient’s jaw and its on-screen cone beam computed tomography (CBCT) scan representation, the tag installed on the patient’s jaw must be mapped with the CBCT scan. The mapping of the trackable jaw tag to the CBCT scan is called registration. Traditionally, the patient would have to be CT-scanned with an artificial radiographic marker, also known as “fiducial”, which has to be later identified in the CT images by the navigation system’s software in order to enable the registration.7
The innovative trace registration method (Navident, ClaroNav) eliminates the need for this artificial fiducial body to be present in the image, by replacing it with natural high-contrast surfaces, such as tooth crowns or abutments already present in the image. Therefore, it eliminates the need for patient exposure to a new dedicated CT scan with a fiducial. The level of radiation is an important issue in diagnosis.9,10 This new method also eliminates the need to have a special stent prepared to couple the fiducial or trackable tag to the jaw in a highly stable and repeatable manner, which was previously essential for the performance of accurate navigation.
To treat the maxilla, a pattern tag, or Head-Tracker, is positioned on the patient’s head like glasses with contact points that don’t move with patient muscle contractions or lower jaw movement (Fig. 1). This ensures that the Head-Tracker maintains a stable relationship with the skull, and thus the maxilla. For the mandible, another pattern tag, called Jaw-Tracker, is temporarily connected to one to two teeth using dual-cure composite resin (without etching the teeth to allow for easy removal; Fig. 2). This Jaw-Tracker can also be used for the maxilla instead of the Head-Tracker.
The surgeon chooses four to six identifiable landmarks on structures which are rigidly attached to the jawbone (teeth, abutments) and are easily visible in the CBCT scan. In the next step, the surgeon traces a path on the surface of each one of the marked structures with a tracer tool, also tracked by the camera (Fig. 3). The system collects 100 points on each one of the traced structures, and optimally matches them to the CT image data to register the Head-Tracker or Jaw-Tracker, with the patient’s maxillary or mandibular CBCT scan, respectively.
Advantages of trace registration
The most important advantages of the trace based over the fiducial/stent-based registration method are:
- No need to design and fabricate a stent or guide in advance, eliminating the associated preparation time and effort, as well as the potential risk for inaccuracy due to improper seating of the stent during the scan or procedure.
- An existing CBCT scan can be used, there is no need for a special scan with stent and fiducial(s). The scan may be taken in full occlusion resulting in easier digital prosthetic planning.
- No stent or guide is in the patients’ mouth during treatment, allowing the same access space in the oral cavity during surgery as with a freehand approach.
Possible limitations
- At least four high-contrast structures fixed to the jaw bone must be available and accessible for tracing. These can be teeth, abutments, bone screws, orthodontic brackets and wires, or similar structures. With fully edentulous patients, regions of the jaw bone itself may be exposed and used as landmark regions.
- Each of the traced regions should not have changed in appearance or location relative to the jaw bone since the scan was taken. If guidance is critical and changes to the jaw such as changes in teeth position are a concern, a fresh scan prior to surgery is advised.
Case presentation
The treated patient was a 54-year-old female with a removable prosthesis, who wished to have a fixed solution. The patient was a non-smoker without medical problems. Intraoral examination revealed the absence of tooth #24 and bone resorption where the teeth had been extracted.
Planning procedure
A CBCT scan was taken without any radiographic marker (Fig. 4). The images were taken with a Carestream 8100 3D (Henry Schein). The field of view used was 80 x 90mm and a voxel size of 150μm. The exposition parameters were 84kV and 4mA. The images were analysed and converted into DICOM files and then converted into a 3-D virtual model by the Navident software. A virtual crown and implant were planned to have 2mm of buccal bone and a restorative space at the centre of the crown (Fig. 5). The virtual implant planning was then modified creating an angulation of six degrees in vestibular direction, so the surgeon would be guided to initiate bone preparation with a six-degree vestibular angulation (Fig. 6).
Surgical procedure
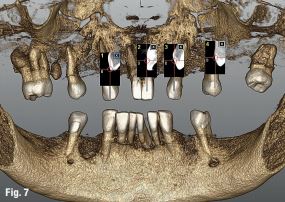
Local anaesthesia was performed in region #24 and aseptic and sterile conditions were applied to prevent infections. The Head-Tracker was positioned and inspected for stability. Trace registration was performed by marking four landmarks on teeth using a panoramic 3-D presentation of the jaw, then tracing the landmark regions with the tracer tool while the camera and software collected 100 points on each tooth (Fig. 7). Navident automatically registered the Head-Tracker with the patient’s maxillary CBCT scan based on the collected points.
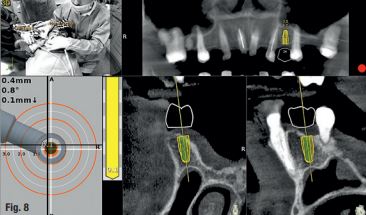
In the next step, drill calibration and accuracy check were performed before the use of each drill. A small incision for a reduced flap was made. All osteotomies were performed at 800 rpm. The virtual implant angulation was pre-surgically modified six degrees in vestibular direction, so the osteotomy could be initiated on that angle. Next, the virtual implant was repositioned intraoperatively on the Navident software and the rest of the site preparation was carried out according to the final angulation with osseodensification drills (Fig. 8). The osteotomies were made with two angulations and tracked in real time and the same procedure was applied for the implant insertion. A cover screw was attached before the surgical area was sutured. The patient reported no discomfort during the surgery.
Postoperative evaluation
The patient reported no pain or swelling. Radiographic and clinical images were taken with a direction indicator screwed onto the implant. The postoperative evaluation showed that the position of the implant exactly corresponded to the virtual planning made beforehand (Figs. 9–14).
Conclusion
The patient benefited from a treatment with a reduced flap and precise implant placement using dynamic navigation technology with an innovative trace registration method. Trace registration in combination with dynamic navigation proved to be a valid technology for osteotomy preparations and implant placement. It does not require a dedicated CT with a radiographic marker nor the fabrication of a stent or clip. When clips or stents are difficult or impossible to use, or even in every dental patient case, trace registration can be the best solution for dynamic navigation implant placement.
References
1. Somogyi-Ganss E, Holmes HI, Jokstad A. Accuracy of a novel prototype dynamic computer-assisted surgery system. Clin Oral Implants Res. 2015 Aug;26(8):882-90.doi: 10.1111/clr.12414.
2. Block MS, Emery RW, Lank K, Ryan J. Implant Placement Accuracy Using Dynamic Navigation. Int J Oral Maxillofac Implants Surg. 2017; 75:1377-1386.
3. Umapathhy T, Jayam C, Anila BS. Overview of surgical guides for implant therapy. Journal of Dental Implants, 2015 Jan-Jun; 5(1):48-52.
4. Kate MA, Plaskar S, Kappor P. Implant failure: A dentist’s nightmare. J Dent Implant 2016; 6:51-56.
5. Palma-Carrió C, Maestre-Ferrin l, Peñarrocha-Oltra D, Peñarrocha-Dago MA, Peñarrocha-Diago M. Risk factors associated with early failure of dental implants. A literature review. Med Oral Patol Oral Cir Bucal. 2011 Jul; 16(4):514-517.
6. Borisov R. Radiological templates and CAD/CAM surgical guides. A literature review. J of IMAB. 2016 Jul-Sep; 22(3):1285-1295.
7. D’ahese J, Ackhurst J. Bruyn H. Immediate loading with dynamic navigation implant surgery. International magazine of oral implantology. 2015; 3:34-37.
8. D’haese J, Van De Velde T, Komiyama A, Hultin M, De Bruyn H. Accuracy and Complications Using Computer-Designed Stereolithographic Surgical Guides for Oral Rehabilitation by Means of Dental Implants: A Review of the Literature. Cl in Impl Dent Rel Res 2012; 14:321–335.
9. Dula K, Mini R, van der Stelt PF, Buser D. The Radiographic Assessment of Implant Patients: Decision-making Criteria. International Journal of Oral & Maxillofacial Implants. 2001 Jan/Feb; 16(1):80-89.
10. Uysal H, Basal N. Dynamic navigation in fully edentulous maxilla. International magazine of oral implantology 2017; 3:38-41.
Contact
Dr Ricardo Henriques
Private Practice
R. S. Martinho, 423 – R/C
4505-164 Argoncilhe, Portugal
[email protected]